Endocrine Hypertension
Yang group
One hundred million people worldwide may have primary aldosteronism, a potentially curable hormonal cause of high blood pressure, yet the vast majority do not know It. The Endocrine Hypertension Group works with clinicians, scientists, consumers and change-makers around the world to ensure that every affected person with primary aldosteronism will receive timely diagnosis and life-saving treatment.
Research group
Overview
Hypertension is a leading risk factor for death and disability globally. Close to six million Australian adults, or 34 per cent of the population, are affected. To reduce the burden of disease associated with hypertension, better diagnosis of a treatable and potentially curable cause of hypertension – primary aldosteronism (PA), or Conn Syndrome – is needed.
The Yang group is
- Studying large birth cohorts to understand the origins of this disease
- Surveying clinicians and consumers to Identify barriers to diagnosis
- Testing novel interventions in primary and tertiary care settings to improve and simplify the diagnostic process
- Testing new or repurposed drugs for the optimal treatment of PA.
PA is caused by excessive aldosterone production from either one or both adrenal glands. It can be effectively treated with aldosterone-blocking medications or cured with surgery, if there is a unilateral aldosterone-producing adrenal adenoma.
While previously considered as rare, PA has been found to affect 5-15 per cent of hypertensive patients in primary care and up to 30 per cent of patients with resistant hypertension. However, PA is not routinely screened for. Half a million hypertensive Australians, and far more globally, may be missing out on targeted treatment or a cure for their hypertension.
A missed or delayed PA diagnosis is detrimental. Patients with PA are two to four times more likely to suffer from heart disease, stroke, atrial fibrillation and chronic kidney disease compared to patients with essential hypertension. These complications can be prevented with early diagnosis and targeted treatment.
After screening, the diagnosis of PA and accurate subtyping remains challenging, time-consuming, and costly, involving hospital stays.
The team’s goal is to diagnose every patient who has primary aldosteronism, in all communities including the disadvantaged populations, in the most time-efficient and cost-effective manner and offer efficacious targeted management with minimal side effects.
“PA was discovered more than 70 years ago, and yet people are still struggling with Its detection and treatment – we need to do better, for the sake of healthier hearts, kidneys and brains.” A/Prof Yang
Diseases we research
Areas of focus
- Evaluating the cost-effectiveness of diagnosing and treating primary aldosteronism
- Identification of novel biomarkers of primary aldosteronism
- Exploring endocrine hypertension in Indigenous populations
- Discovering barriers to testing for primary aldosteronism
- Identifying the origins of primary aldosteronism: when and how does it start?
Research Group Head | Associate Professor Jun Yang
Primary Aldosteronism (PA), or Conn Syndrome, is the most commonly under-diagnosed cause of high blood pressure affecting millions of people. My goal is to facilitate the diagnosis of every case of PA and make treatment widely available to all communities including the disadvantaged.

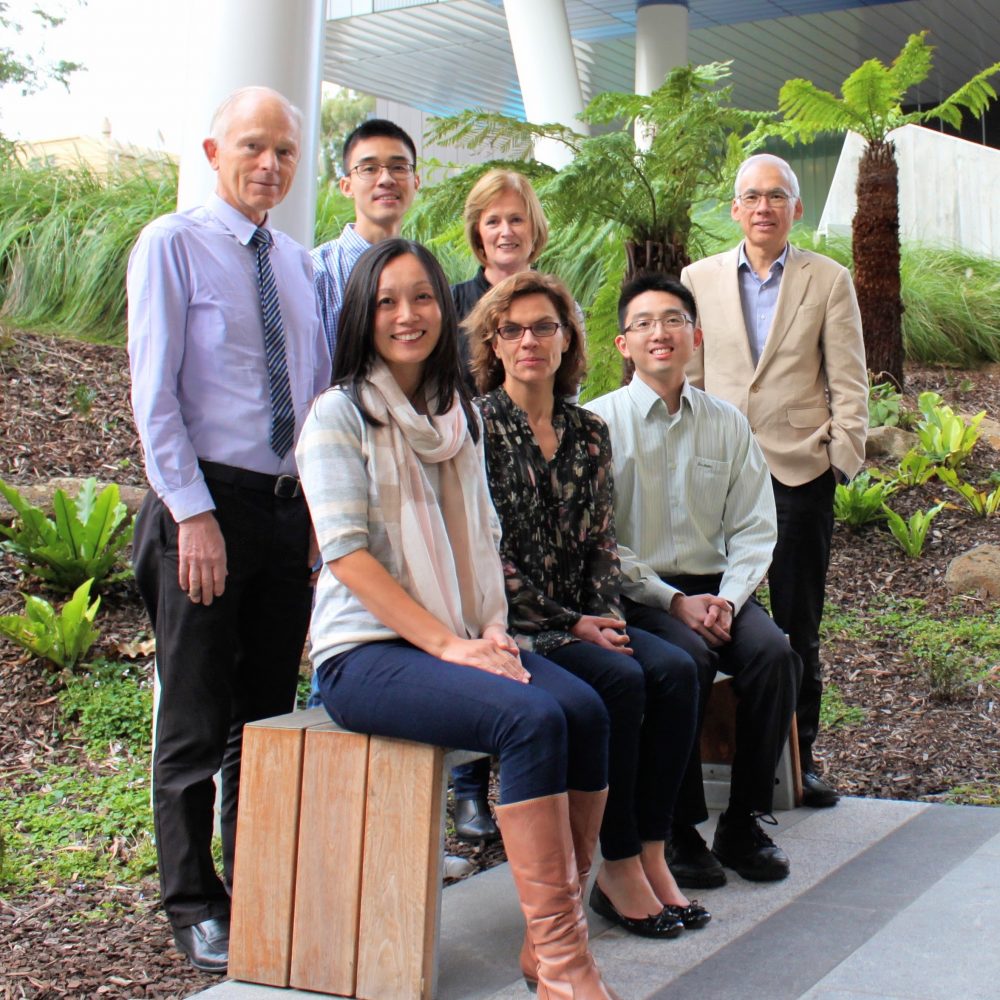
Meet the team

 Dr Jimmy Shen
Senior Research Scientist
Dr Jimmy Shen
Senior Research Scientist
 Dr Renata Libianto
Postdoctoral Scientist
Dr Renata Libianto
Postdoctoral Scientist
 Muhammad Akram
Research Support Staff
Muhammad Akram
Research Support Staff
 StellaMay Gwini
Research Support Staff
StellaMay Gwini
Research Support Staff
 Catherine He
Research Support Staff
Catherine He
Research Support Staff
 Dr Linghan Jia
Research Support Staff
Dr Linghan Jia
Research Support Staff
 Michelle Kouspou
Research Support Staff
Michelle Kouspou
Research Support Staff
 Shanshan Lu-Shirzad
Research Support Staff
Shanshan Lu-Shirzad
Research Support Staff
 James Morgan
Research Support Staff
James Morgan
Research Support Staff
 Peta Nuttall
Research Support Staff
Peta Nuttall
Research Support Staff
 Dr Sharmin Jahan
PhD Student
Dr Sharmin Jahan
PhD Student
 Nikshay Karthigan
PhD Student
Nikshay Karthigan
PhD Student
 Dr Josephine McCarthy
PhD Student
Dr Josephine McCarthy
PhD Student
 Dr Elisabeth Ng
PhD Student
Dr Elisabeth Ng
PhD Student
 Dr Sonali Shah
PhD Student
Dr Sonali Shah
PhD Student
News from the lab
Student opportunities

Collaborators

Publication highlights



