Spread of cancers to bone
Spread of cancers to bone is a Research Project for the Metabolic Bone Research Research Group, under the Centre for Endocrinology and Metabolism.
Targeting activin to counteract life-threatening cancer cachexia
 This project aims to identify why some cancers, particularly those of the breast, have a predilection to bone, and determine mechanisms to limit tumour growth in bone as well as to understand the biology and intra-nuclear actions of PTHrP, including its actions on breast cancers. We are also working to understand the role of bone microenvironment in changes to breast cancer cells and the action of breast cancer-derived factors on osteoblasts and osteoclasts. In understanding metastasis of breast cancer to bone, we hope to identify existing breast cancer therapies shown to contribute to tumour bone invasive ability.
This project aims to identify why some cancers, particularly those of the breast, have a predilection to bone, and determine mechanisms to limit tumour growth in bone as well as to understand the biology and intra-nuclear actions of PTHrP, including its actions on breast cancers. We are also working to understand the role of bone microenvironment in changes to breast cancer cells and the action of breast cancer-derived factors on osteoblasts and osteoclasts. In understanding metastasis of breast cancer to bone, we hope to identify existing breast cancer therapies shown to contribute to tumour bone invasive ability.
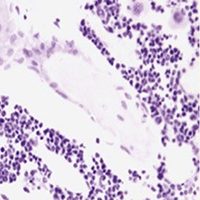
Breast and other tumours, including kidney and lung cancers may metastasise to bone where they establish and grow, typically resulting in local bone breakdown – termed an osteolytic metastasis. Prostate cancers also spread to bone, but result not in destruction but in massive bone formation – an osteoblastic metastasis.
Both types of metastasis are associated with considerable pain and, in the case of osteolytic metastases, fractures result from the weakened bone structure. We have examined how breast cancers result in osteolytic metastases and determined that this is in part due to parathyroid hormone-related protein (PTHrP) production by the tumour, which stimulates the local normal bone cells to form osteoclast cells.
Bone is removed as a result of osteoclast formation, releasing some hormones that are normally stored within the bone. This includes the hormone TGF-β, which powerfully stimulates the tumor cells to produce more PTHrP, and this sets up a vicious cycle of more bone destruction leading to more PTHrP, and so on.
The interaction of these cell types with the bone matrix facilitates the establishment of a vicious cycle for bone destruction. We have identified a number of agents that block the progression of this cycle, we are evaluating these in model systems.
Our studies have revealed that, while effective at shrinking tumours in mice, anti-cancer drug 17-AAG can cause bone damage and increase the growth of breast cancer cells that have spread to the bone. We have found that 17-AAG induces a stress response in osteoclasts which, when blocked, reduces osteoclast formation. Our research has identified a number of key targets of this stress response, which appear to be linked to osteoclast formation. We are now working to translate these findings into pre-clinical models.
Collaborators:
Associate Professor John T. Price

