Endometrial Stem Cell Biology
Professor Caroline Gargett leads a diverse team of scientists in the Endometrial Stem Cell Biology Group. They work on two broad themes of women’s health – pelvic organ prolapse and endometriosis/gynaecological disease.
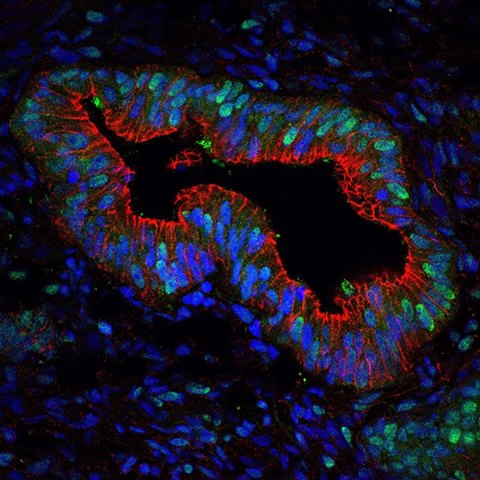
Endometrial stem cells
Overview
Pelvic Organ Prolapse is an extremely common condition that results from herniation of pelvic organs into the vagina due to injury experienced during childbirth. Pelvic Organ Prolapse causes difficulty in passing urine, affects bowel motions and can result in sexual problems. Endometriosis is a serious chronic disease, that affects 10% of people who menstruate, where endometrial tissue grows outside the uterus. It causes severe pain and infertility and current treatments are suboptimal.
The Endometrial Stem Cell Biology Group’s discovery and characterisation of endometrial stem/progenitor cells in the highly regenerative lining of the uterus (endometrium) of human, sheep and mice has formed the basis of a wide range of projects in women’s health. Central to these is the investigation of endometrial stem/progenitor cells;
- As a potential therapy for pelvic organ prolapse and
- Their role in endometriosis/adenomyosis and other gynaecological diseases.
The Endometrial Stem Cell Biology Group’s previous application of endometrial stem/progenitor cell biology has led to the following.
Endometriosis and gynaecological disease – contributions to the field
- The landmark discovery that endometrial stem/progenitor cells are shed in menstrual blood and gain access to the pelvic cavity during retrograde menstruation, and are therefore putative candidates for the cellular origins of endometriotic lesions.
- Characterisation of minimal cycle-to-cycle variation in menstrual fluid parameters in women, allowing development of indicative ranges for the use of menstrual fluid as a non-invasive diagnostic tool
- Characterisation of the role of telomerase in menstrual repair and sonic hedgehog signalling in the pathogenesis of endometriosis using pre-clinical mouse models (developed by Dr Fiona Cousins).
- Characterisation of Type I interferon, interferon epsilon in the pathogenesis of endometriosis, using pre-clinical models and in vitro 2D/3D culture methods.
Pelvic organ prolapse – contributions to the field
The utility of endometrial MSC combined with novel scaffold non-degradable biomaterials developed with CSIRO collaborators and more recently degradable nanomaterials by team member Dr Shayanti Mukherjee as a cell-based therapy for treating and preventing Pelvic Organ Prolapse. Our tissue engineering approach for vaginal surgical repair shows promise in a rat model and in a sheep vaginal surgery model for pre-clinical studies. This interdisciplinary research also includes the following
- Using a small molecule to maintain stemness of endometrial MSC during culture expansion, producing a reproducible cell product for clinical use. Combined RNAseq and ATACseq has discovered the mechanism involved and the research has been applied to placental, menstrual blood, adipose and bone marrow MSC
- The identification of parous sheep with weakened vaginal walls by adapting clinical approaches used in humans for selection of sheep for preclinical assessment of tissue engineering constructs in vaginal surgery
- Development of a simple two step surgical procedure for insertion of mesh and endometrial MSC in an ovine model of Pelvic Organ Prolapse
- The development of a secondary prevention strategy for treating women soon after childbirth with their own endometrial MSC and novel nanobiomaterials for local delivery of cells to prevent Pelvic Organ Prolapse occurring later in life
- The immunomodulatory properties of human endometrial MSC. Similar to bone marrow MSC, endometrial MSC show anti-inflammatory, immunomodulatory properties and promote wound healing in culture and in mouse, rat and ovine models
- Development of a novel pressure sensor device using fibre optics technology by collaborators from Flinders University has been trialled in women to more precisely diagnose areas of vaginal wall weakness.
Endometrial Stem Cell Biology Research group projects
Endometriosis/gynaecological disease
- RNAseq on purified populations of endometrial stem/progenitor cells is being examined to identify differences between women with endometriosis that allow the stem/progenitor cells to implant and grow in the pelvis and normal women.
- Use of 3D organoid cultures to investigate the properties and signalling pathways used by human and mouse endometrial epithelial progenitor cells.
- Role of immune modulation in development of endometriosis.
- The role of endometrial stem/ progenitor cells in stillbirth.
- Investigation of neonatal uterine bleeding as a potential biomarker of adolescent endometriosis.
- The role of endometrial stem/ progenitor cells in endometrial-related infertility where the endometrium fails to support embryo implantation particularly in women with Recurrent Implantation Failure undergoing IVF procedures.
Pelvic organ prolapse
- Development of a large animal (sheep) pre-clinical model of birth-induced injury to assess the efficacy of autologous endometrial MSC as a cell-based therapy to prevent Pelvic Organ Prolapse.
- Developing potency assays and release criteria for autologous endometrial MSC in preparation for clinical use.
- Nanotechnology and tissue engineering strategies for preventing and treating Pelvic Floor Disorders.
- Use of 3D printing approaches to assess design principles influencing the efficacy of degradable scaffolds for delivering MSC to damaged vaginal tissue and promote healing.
Diseases we research
Research Group Head | Professor Caroline Gargett
Pelvic organ prolapse (POP) and endometriosis are two areas of women’s health that have a debilitating effects on women’s lives. I lead a diverse team of scientists working on these issues to improve diagnosis and treatment options for the women.

Meet the team

 Dr Fiona Cousins
Research Scientist
Dr Fiona Cousins
Research Scientist
 Dr Harriet Fitzgerald
Postdoctoral Scientist
Dr Harriet Fitzgerald
Postdoctoral Scientist
 Dr Shanti Gurung
Postdoctoral Scientist
Dr Shanti Gurung
Postdoctoral Scientist
 Dr Thomas Tapmeier
Honorary Research Associate
Dr Thomas Tapmeier
Honorary Research Associate
 Professor Jerome Werkmeister
Honorary Research Associate
Professor Jerome Werkmeister
Honorary Research Associate
 Elizabeth Marquez-Garcia
Research Support Staff
Elizabeth Marquez-Garcia
Research Support Staff
 Dr Kjiana Schwab
Research Support Staff
Dr Kjiana Schwab
Research Support Staff
 Emily Brennan
PhD Student
Emily Brennan
PhD Student
 Dinasha Wimalasiri
PhD Student
Dinasha Wimalasiri
PhD Student
 Kirstin Tindal
PhD Student
Kirstin Tindal
PhD Student
 Abi Cameron
Honours Student
Abi Cameron
Honours Student
 Claire Davison
Honours Student
Claire Davison
Honours Student
 Jenna Douglas
Honours Student
Jenna Douglas
Honours Student
 Shreya Mago
Honours Student
Shreya Mago
Honours Student
News from the lab
Student opportunities

Publication highlights


