How the immune system contributes to stomach cancer
By Rob Clancy, staff writer
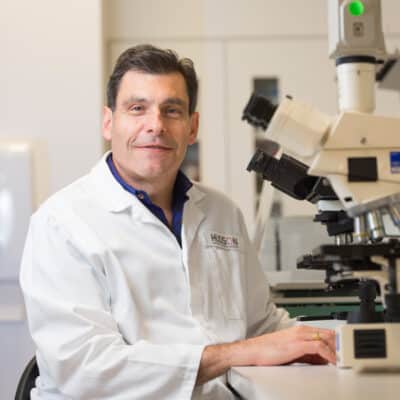
Researchers aim to beat stomach cancer at its own game by identifying modulators of the innate immune system that drive it and applying the brakes before cancer takes hold. In 2021, Professor Brendan Jenkins and Dr Ruby Dawson challenged conventional thinking about how stomach cancer forms – the answers have created a paradigm shift in scientific thinking around how the immune system contributes to the development of stomach cancer.

Stomach cancer is the third most lethal cancer worldwide, with a five-year survival rate of less than 30 per cent.
Rethinking stomach cancer
Most stomach cancers are caused by uncontrolled activation of two arms of the immune system: the innate or first line of defence, and the adaptive or slower specific immune response. To date, scientists have focused on adaptive immune-based pathways and treatments, but these have yielded limited clinical results.
“To find new treatments we must identify new immune system genes to target, so we looked outside the box at the underexplored innate immune system,” says Prof Jenkins.
Improving stomach cancer treatment and survivial
The team’s discovery, published in the prestigious Gut journal, identified a critical contributor to stomach cancer development, namely the underexplored innate immune system protein, AIM2.
“This is a substantial advance in the molecular mechanisms underlying stomach cancer, offering enormous potential to dramatically improve treatments and stomach cancer survival,” said Professor Brendan Jenkins.
Stomach cancer immune trigger found
“If you think of a cell as a finely tuned orchestra with instruments playing in harmony and taking cues from each other, we discovered that AIM2 is playing way too loud. This causes chaos that triggers cancer in the cell. We aim to restore the harmony,” says Dr Dawson.
“Targeting immune regulators like AIM2 and potentially other related immune system regulators is an untapped strategy; it gives scientists new targets to use for drugs and the potential for a clearer picture of a patient’s prognosis,” says Prof Jenkins.
Potential for improved patient outcomes
The discovery provides a major advance in the fundamental understanding of the molecular mechanisms governing stomach cancer and has enormous potential to influence future clinical management and dramatically improve patient outcomes.
Collaborators | Monash Health; Cancer Research Institute, Japan; Duke-NUS Graduate Medical School, Singapore; Kanazawa University, Japan; National Cancer Institute, USA
Funders | National Health and Medical Research Council (NHMRC)
Contact us
Hudson Institute communications
t: + 61 3 8572 2761
e: communications@hudson.org.au
In this article
About Hudson Institute
Hudson Institute’ s research programs deliver in five areas of medical need – inflammation, cancer, reproductive health, newborn health, and hormones and health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”