Disease of moving parts: examining the puzzle of cancer
By Hudson Institute communications
For more than 50 years, the idea that cancer is caused by abnormal genes has been driving cancer research and treatment.

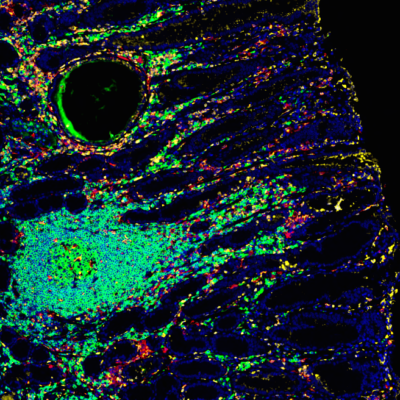
Now, discovery research into epigenetics (how genes are switched on and off), inflammation and tissue organisation (the interaction between cells and organs) is leading scientists to acknowledge that just like the human body, cancer is made up of many moving parts and causes. Genes alone do not hold all the answers.
“Cancer is not one disease, but many,” Dr Elizabeth Sigston, a Hudson Institute of Medical Research PhD student and Monash Health ear nose and throat surgeon, who specialises in head and neck cancers, says.
A new framework developed by Dr Sigston enables scientists and clinicians to critically re-examine theories for what causes cancer in a way that makes them complementary rather than competing, to pave the way for improved treatment.
“Understanding cancer is like understanding a symphony: while each part can be studied in detail, ultimately it is how all the parts come together that creates the music that is heard. This framework provides the conductor’s score,” she says.
Cancer is one of the leading causes of death in Australia. Around one in three Australian men and one in four Australian women will be diagnosed with cancer before the age of 75.
New framework for cancer treatment
‘An Emergence Framework of Carcinogenesis’ is a systems -based framework developed by Dr Sigston as part of her PhD at Hudson Institute, supervised by Professor Bryan Williams. It has been published in the journal Frontiers in Oncology.
Dr Sigston says the framework can be applied by researchers or clinicians to start with either a clinical question or science discovery to better understand cancer. In her own research, she is using the framework to identify biomarkers in tongue and oral cancers that could predict the risk of recurrence and identify early patients who would potentially benefit from immunotherapies.
The framework synthesises current concepts of cancer development into 12 principles for researchers, clinicians, institutions and funding bodies involved in researching and treating cancer.
“This framework allows us to take a step back from the details and see how the details fit together and impact on where cancer really matters, in people,” Dr Sigston, who is also a lecturer in Monash University’s Department of Surgery, says.
“It allows for seemingly contradictory findings to fit side-by-side as pieces of the puzzle and provides a roadmap for translation research.”
Targeted therapies come from bench to bedside
“This new framework provides a unified paradigm for understanding cancer and a practical link between the bedside and benchtop, aiding translational research,” Dr Sigston, says.
“Understanding each cancer as a complex system opens the doorway to not only understanding each cancer, but how each cancer may differ in different people, paving the way for more targeted therapies and better treatment outcomes.”
This research was generously supported by a Project Grant 2007 from the Garnett Passe and Rodney Williams Memorial Fund and funding from the Department of Surgery (Monash Medical Centre), Monash University
Contact us
Hudson Institute communications
t: + 61 3 8572 2697
e: communications@hudson.org.au
About Hudson Institute
Hudson Institute’ s research programs deliver in five areas of medical need – inflammation, cancer, reproductive health, newborn health, and hormones and health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”